by TOM PAGONIS, DDS, MS
Introduction
The fundamental aim of root canal sealers with the combination of gutta-percha is to prevent reinfection by providing an adequate seal against ingress of bacteria and their toxins.(1) The importance of sealers and their function has created a substantial body of literature on their biological, physical, and chemical properties. These materials have been reviewed and are categorized primarily by their main constituents, such as calcium hydroxide, zinc oxide eugenol, resin, silicone, glass ionomer, and bioceramic –based components.(2) While the core functions of root canal sealers have largely remained unchanged, contemporary endodontic treatment protocols have seen the emergence of bioceramic sealers as the material of choice. These ceramic-based biomaterials contain both bioactive components such as calcium phosphate and bioinert components such as zirconia and alumina. A significant advantage of these advanced biomaterials is that they are biocompatible due to material alkalinity and osteoconductive properties. This is of particular importance when considering the possible inadvertent extrusion of root canal sealers during non-surgical endodontic procedures. Secondly, the physiochemical and biological properties of bioceramic sealers promote a specific interaction with dentin whereby sealer minerals (i.e. carbonate, calcium, and silica) are incorporated with intertubular dentin. This creates improved bonding at the dentin-sealer interface.(3)
A new generation, advanced bioceramic sealer that has been extensively studied is now available in the U.S. market. This newly available sealer known as Endoseal MTA (Maruchi, Wonju, Korea) (Figure 1) offers clear advantages over other bioceramic sealers.
Figure 1
Evaluating novel Endoseal MTA Bioceramic Technology
Endoseal MTA directly addresses setting time and introduces a remarkably shortened and clinically welcome rapid setting time especially when compared to other bioceramic sealers. There appears to be a universal acknowledgment by both clinicians and manufacturers that setting times need to be markedly improved. Manufacturers have made several attempts to address this problem by introducing chemical adjuncts or accelerators to existing formulations. This approach has not worked and in fact, has produced undesirable biological and physical effects. (4)
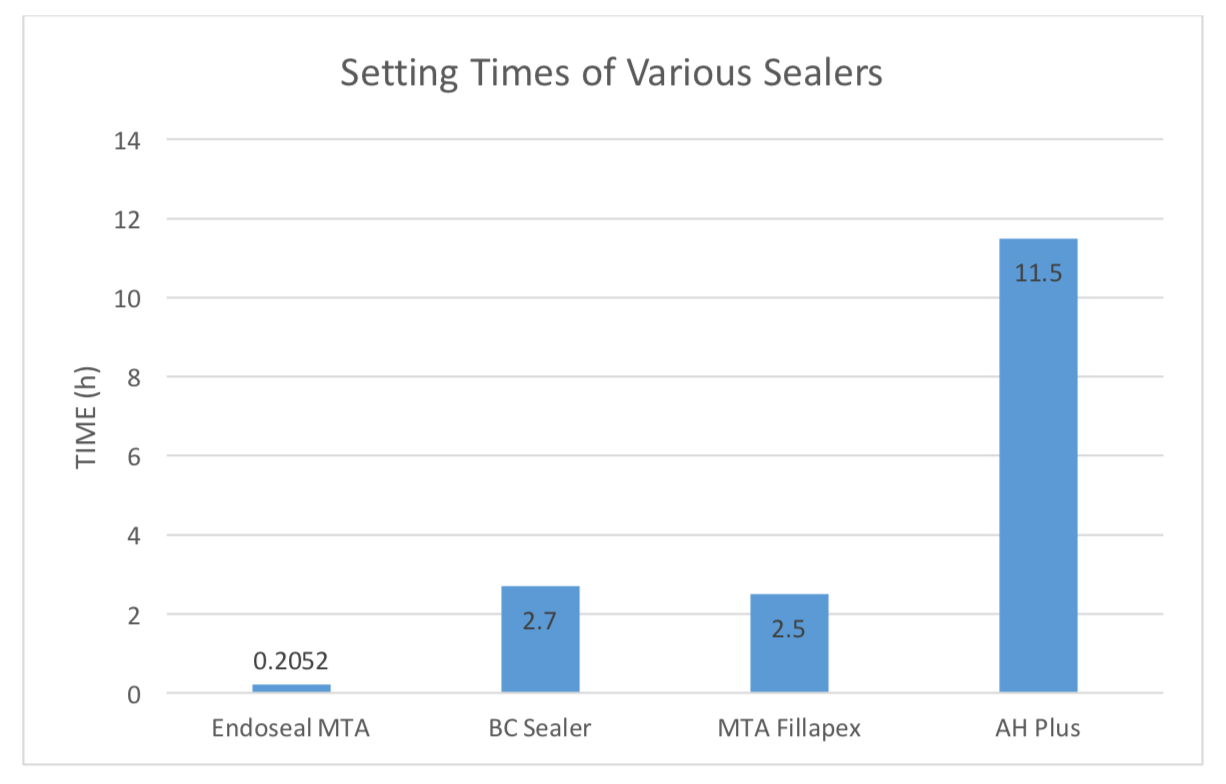
Based upon a novel pozzolan derived cement, Endodoseal MTA provides faster setting times through its chemical and physical composition rather than through the addition of chemical accelerators. Small particles of pozzolon cement can best be described as a siliceous or siliceous and aluminous material which on their own do not have cementitious value. But the Endodoseal MTA proprietary formulation, which utilizes finely divided particles, acquires cementitious properties in the presence of water when reacting with calcium hydroxide at room temperature. Taken together with all the Endodoseal MTA components, there is a cascade of pozzolanic reactions which can essentially be divided into two main processes. The first relates to the gradual decrease in calcium hydroxide which is advantageous if one considers that calcium hydroxide will have deleterious effects on mechanical properties and on material durability. Secondly, the pozzolanic reaction is characterized by an increased formation of calcium silicate hydrate and calcium hydrate stable crystals. The significance of this crystal development coupled with the decrease in free calcium effectively contributes to material durability. Finally, there is increased surface contact with the ultrastructure of smaller sized particles with the accompanying mixing liquid. This provides a much more favorable rapid setting time with ease of handling. In a comparative study utilizing EndoSequence BC sealer Brassler), MTA Fillapex (Angelus Industria de Produtos Odontologicos S/A, Londrina, Brazil) and AH Plus (Dentsply, DeTrey, Konstanz, Germany), Endoseal MTA set in 12.31 min (0.2052 hours) compared to 2.7 hours for BC sealer (Table 1).(5)
Table 1 Setting times of ENDOSEAL MTA and various root canal sealers
A separate study showed that EndoSequence BC sealer did not set in humid incubator conditions – even after one month. While a vastly improved and faster setting time distinguishes Endodoseal MTA, the material offers other attractive characteristics when compared with other bioceramic sealer products.
Choosing Endoseal MTA Bioceramic Root Canal Sealer
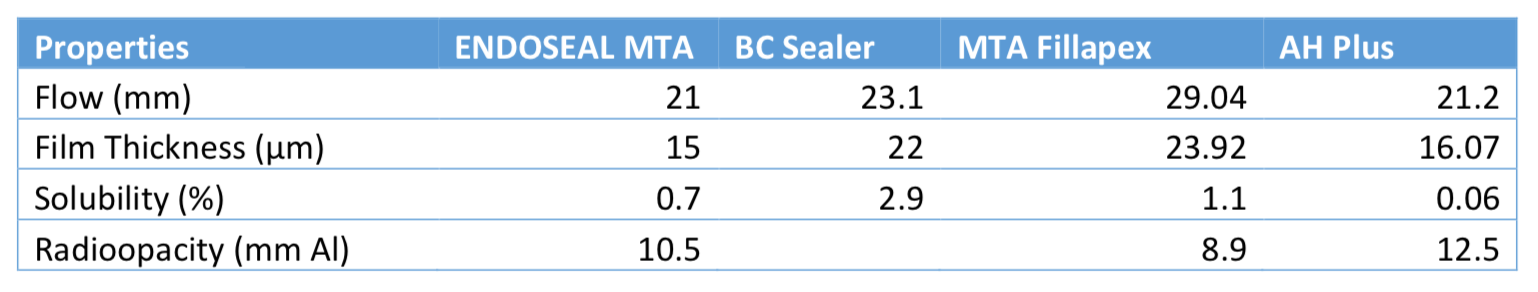
While Endoseal MTA possesses clear advantages with a rapid setting time and ease of handling, it is important to evaluate other parameters in choosing Endodoseal MTA (Table 2).
Table 2 Properties of ENDOSEAL MTA and various root canal sealers
Biocompatibility and Biomineralization. Biocompatibility is typically assessed through cytotoxicity studies on cell line survival of periradicular constituent cells such as osteoblasts, periodontal ligament cells or other cell lines. As previously mentioned, this is a hallmark characteristic of bioceramic sealers. When evaluating cell morphology with MC3T3-E1 cells, or when evaluating tissue histology after experimental tissue implantation in standard lab animals Endoseal MTA displayed very favorable biocompatibility. Pozzolan-based Endoseal MTA also exhibits significant dynamic intratubular biomineralization beyond the dentinal tubule sealer tag in ex vivo SEM studies.(6)
Antimicrobial Properties Root canal sealers are tasked with both overcoming the limitations of gutta percha by filling spaces between obturation material and dentinal walls while providing antibacterial properties to residual bacteria. In an independent in vitro laboratory study comparing the antibacterial activity of Endoseal MTA, EndoSequence BC sealer, AH Plus, Sealapex, and Tubli-seal it was determined that Endoseal MTA showed antibacterial activity against not only the Gram-negative bacteria but also exhibited substantial antimicrobial activity to E. faecalis (Gram-positive bacteria). This was in stark contrast to EndoSequence BC sealer which exhibited a weak antibacterial effect on all bacteria studied. In addition, when compared to Endosequence BC sealer, it was determined through X-ray fluorescence analysis that Endoseal MTA contained a greater profile and greater quantities of oxide compounds such as Al2O3, Fe2O3, Mgo, Na2O, NiO, and SO2. These oxide compounds are known to exhibit strong antimicrobial activity. (7)
Flow. If one considers the complex anatomy of the root canal system, flow is an important property when addressing the sealer ability to seal fins, isthmuses, voids, and inaccessible patent accessory canals. Utilizing contact angle as an experimental indicator of wetting ability, Endoseal MTA performed extremely well in a comparative study with other bioceramic sealers and with an epoxy-resin-based sealer. This characteristic is important because it is related to adequate material flow. Endoseal MTA exhibits excellent wetting and adhesion properties which is a critical requirement when considering both sealer binding ability between dental walls and filling material along with penetrability in anatomically complex areas of the root canal system.
Tooth Discoloration. The introduction of this novel MTA aggregate root canal sealer warrants an examination of tooth discoloration potential. In vitro studies utilizing standardized bovine tooth samples showed that Endoseal MTA, when compared to both AH Plus and conventional MTA (ProRoot; Dentsply, Tulsa, OK, USA) showed less discoloration than conventional MTA and no significant difference in brightness change or total color change when compared to AH Plus and control.(8)
Radiopacity. Sufficient radiopacity continues to be an important parameter for root canal sealers as a means to distinguish from radiographic anatomical structures during endodontic clinical procedures. In vitro radiographic studies of Endoseal MTA utilizing graduated 1 mm thick aluminum step-wedge increments showed statistically higher values and greater radiopacity while MTA Fillapex showed statistically lower values in comparison to the other evaluated sealers.(8)
Conclusion
Collectively, the present study indicates that physical and chemical characteristics of Endoseal MTA make this material a leader among bioceramic sealers in the arena of biomineralization, biocompatibility, sealing ability, antimicrobial activity, and radiopacity. From a clinical setting, it provides a significant improvement with very favorable flow characteristics and significantly shortened setting time making it a very Dentist-friendly material. The authors believe and suggest that Endoseal MTA should be the bioceramic sealer of choice in endodontic therapy.
References
1. Kaur A, Shah N, Logani A, Mishra N. Biotoxicity of commonly used root canal sealers: a meta-analysis. Journal of Conservative Dentistry 2015;18(2):83-88.
2. Orstavik D. Materials used for root canal obturation: technical, biological and clinical testing. Endodontics Topics 2005;12(1):25-38.
3. Al-Haddad A, Che Ab Aziz ZA. Bioceramic-Based Root Canal Sealers: A Review. Int J Biomater 2016;2016:9753210.
4. Bin-Na L, Yun-Chan H, Ji-Hyun J, Hoon-Sang C, In-Nam H, So-Young Y, et al. Improvement of the properties of mineral trioxide aggregate by mixing with hydration accelerators. J Endod 2011(37):1433-1438.
5. Lee JK, Kwak SW, Ha JH, Lee W, Kim HC. Physicochemical Properties of Epoxy Resin-Based and Bioceramic-Based Root Canal Sealers. Bioinorg Chem Appl 2017;2017:2582849.
6. Yoo YJ, Baek SH, Kum KY, Shon WJ, Woo KM, Lee W. Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning 2016;38(1):50-56.
7. Lim ES, Park YB, Kwon YS, Shon WJ, Lee KW, Min KS. Physical properties and biocompatibility of an injectable calcium-silicate-based root canal sealer: in vitro and in vivo study. BMC oral health 2015;15(1):129.
8. Lee DS, Lim MJ, Choi Y, Rosa V, Hong CU, Min KS. Tooth discoloration induced by a novel mineral trioxide aggregate-based root canal sealer. European journal of dentistry 2016;10(3):403-407.


 Figure 1
Figure 1